BIMONTHLY EXAM
26 year old woman with complaints of altered sensorium somce 1 day,headache since 8 days,fever and vomitings since 4 days
More here: https://harikachindam7.blogspot.com/2020/12/26-year-old-female-with-complaints-of.html
Case presentation links:
https://youtu.be/fz9Jssoc-mA
https://youtu.be/d4lLX04oL8
https://youtu.be/CSCxw2zp7Oc
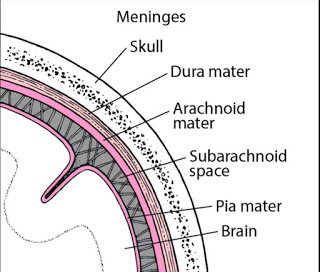
a). What is the problem representation of this patient and what is the anatomical localization for her current problem based on the clinical findings?
problem:
• headache 1 -2 times /week since 1 month and along with neck pain
• both hands small joint pain and later elbow and shoulder involved. she diagnosis as SLE
• she present to causality with altered sensorium and irrelavent talk
• history of vomittings and generalised weakness ,decreased appetite ,unable to walk
• history of low grade fever and joint pain
1. Hyponatremia secondary to SIADH
2. Tubercular meningitis
3. Acute infarct in the left thalamic region
4. SLE with multiple joint pains
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of her problems and current outcomes.
2. Tubercular meningitis
3. Acute infarct in the left thalamic region
4. SLE with multiple joint pains
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of her problems and current outcomes.
According to the patient history,
the etiology mycobacterium tuberculosis,also the CBNAAT done for csf is positive,indicating Tubercular meningitis
To arrive at a diagnosis,for chronic headache CT or MRI is the preferred modality,
MRI was done and it revealed focal acute infarcts in the left thalamus.
Also lumbar puncture was done it revealed normal protein and cell count but the glucose levels were decreased.
sequence of events
Tubercular meningitis (TBM) is a rare condition in patients with systemic lupus erythematosus (SLE). The aim of this study is to describe the clinical characteristics, possible risk factors, and outcomes of SLE patients with TBM. On systematically reviewing medical records from10 SLE patients with TBM admitted to a hospital from December 2008 to December 2018. A total of 100 cases in the same period were randomly selected as controls from SLE inpatients without infection. In patients with TBM, the mean age at presentation was 35.2 years (range 19.8–45.2); the mean duration of SLE was 34.6 months (range 4–84 months).
Patients with TBM had significantly longer SLE duration, higher ESR and CRP level, and lower CD4+ cell counts and albumin level than those without infections (p < 0.05 for all). There were no differences in prednisone dose at the time of symptom onset or cumulative dose over the preceding year between the two groups. Logistic regression analysis showed that patients with a lower CD4+ cell count were more likely to have TBM compared with controls (OR = 3.67, p = 0.020).
TBM should be considered when SLE patients have central nervous system (CNS) symptoms with a longer duration, higher ESR and CRP level, and lower CD4+ cell counts and albumin level, even if the patients are receiving a low prednisone dose,and the patient being studied has a chronic headache and fits into this criteria
c) What is the efficacy of each of the drugs listed in her prior treatment plan that she was following since last two years before she stopped it two weeks back?
. Hydroxychloroquine
.sulfasalazine
. methylprednisolone
.aceclofenac
. Hydroxychloroquine
.sulfasalazine
. methylprednisolone
.aceclofenac
. cholecalciferol
.alandronic acid
. flupirtine
. gabapentin
. methylcobalamine tablets.
1.Why was she given bisphosphonates?
1) Hydroxychloroquine in SLE
“Chloroquine, together with its hydroxyl derivative hydroxychloroquine, was initially used as an antimalarial agent, but is also useful in the treatment of autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus (SLE).
• Chloroquine and hydroxychloroquine are approved for the treatment of SLE and have been shown to reduce the frequency of disease flares (particularly of lupus nephritis), contribute to the maintenance of remission, prolong the onset of disease and reduce the risk of complications.Beyond their immunomodulatory effects in SLE, these agents have also been shown to protect against thrombotic events, improve glucose and lipid profiles, and prevent renal damage,apparently resulting in reduced cardiovascular risk, for which SLE is an independent risk factor”
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7097534/
2)sulfasalazine
Immunosuppressive drug used in the treatment of cutaneous manifestations of lupus.
“Sulfasalazine is an effective agent for chronic discoid lupus erythematosus (CDLE) but the response to treatment is considerably variable between patients and is also unpredictable. The reason for this might relate to differences in metabolism of the drug which is extensively acetylated by the polymorphic enzyme N-acetyltransferase 2 (NAT2). To test this possibility, the N-acetylation phenotype of eleven patients with CDLE and treated by standard doses of sulfasalazine was retrospectively determined by genotyping. A clear-cut difference in the outcome of treatment was observed according to whether the patients were slow acetylators (SA) or rapid acetylators (RA). Eight out of 11 patients responded to treatment with a complete or marked remission of the disease. Seven of them were RA. The three other patients who did not respond at all to the drug were SA. In addition, SA seem to be more prone to toxic events. These findings strongly suggest that the genetic polymorphism of NAT2 is responsible for differences in the response to sulfasalazine in patients with CDLE. Therefore, candidates for sulfasalazine therapy should be genotyped to identify those patients who might benefit from the drug.”
Source: https://journals.lww.com/jpharmacogenetics/Abstract/1997/04000/NAT2_genotyping_and_efficacy_of_sulfasalazine_in.6.aspx
.alandronic acid
. flupirtine
. gabapentin
. methylcobalamine tablets.
1.Why was she given bisphosphonates?
1) Hydroxychloroquine in SLE
“Chloroquine, together with its hydroxyl derivative hydroxychloroquine, was initially used as an antimalarial agent, but is also useful in the treatment of autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus (SLE).
• Chloroquine and hydroxychloroquine are approved for the treatment of SLE and have been shown to reduce the frequency of disease flares (particularly of lupus nephritis), contribute to the maintenance of remission, prolong the onset of disease and reduce the risk of complications.Beyond their immunomodulatory effects in SLE, these agents have also been shown to protect against thrombotic events, improve glucose and lipid profiles, and prevent renal damage,apparently resulting in reduced cardiovascular risk, for which SLE is an independent risk factor”
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7097534/
2)sulfasalazine
Immunosuppressive drug used in the treatment of cutaneous manifestations of lupus.
“Sulfasalazine is an effective agent for chronic discoid lupus erythematosus (CDLE) but the response to treatment is considerably variable between patients and is also unpredictable. The reason for this might relate to differences in metabolism of the drug which is extensively acetylated by the polymorphic enzyme N-acetyltransferase 2 (NAT2). To test this possibility, the N-acetylation phenotype of eleven patients with CDLE and treated by standard doses of sulfasalazine was retrospectively determined by genotyping. A clear-cut difference in the outcome of treatment was observed according to whether the patients were slow acetylators (SA) or rapid acetylators (RA). Eight out of 11 patients responded to treatment with a complete or marked remission of the disease. Seven of them were RA. The three other patients who did not respond at all to the drug were SA. In addition, SA seem to be more prone to toxic events. These findings strongly suggest that the genetic polymorphism of NAT2 is responsible for differences in the response to sulfasalazine in patients with CDLE. Therefore, candidates for sulfasalazine therapy should be genotyped to identify those patients who might benefit from the drug.”
Source: https://journals.lww.com/jpharmacogenetics/Abstract/1997/04000/NAT2_genotyping_and_efficacy_of_sulfasalazine_in.6.aspx
3) Please critically appraise the full text article linked below:
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2796.2003.01233.x
What is the efficacy of aspirin in stroke in your assessment of the evidence provided in the article. Please go through the RCT CASP checklist here https://casp-uk.net/casp-tools-checklists/ and answer the questions mentioned in the checklist in relation to your article.
https://onlinelibrary.wiley.
What is the efficacy of aspirin in stroke in your assessment of the evidence provided in the article. Please go through the RCT CASP checklist here https://casp-uk.net/casp-

The main results of the trial showed that aspirin treatment did not significantly reduce the rate of stroke progression. The progression rate was 15.9% amongst patients treated with aspirin and 16.7% for those on placebo.
The ability to live at home, to walk unaided, or need for further institutionalized care after discharge was not significantly improved in the aspirin group .
RCT CASP checklist:
https://documentcloud.adobe.com/link/review?uri=urn:aaid:scds:US:8d251179-8d1c-435c-803e-0daf96229a3f
4) Please mention your individual learning experiences from this month.
4) Please mention your individual learning experiences from this month.
- Hypothyroidism and kidney failure
- CLD with portal HTN secondary to ? HCV/Alcohol
- AKI on CKD secondary to Urosepsis
- Pericardiocentesis
- Pleural tap
- TB meningitis
5) a) What are the possible reasons for the 36 year old man\"s hypertension and CAD described in the link below since three years? https://vamsikrishna1996.blogspot.com/2021/01/36-year-male-presented-to-casualty-at.html?m=1
The possible reasons for hypertension and cad in the given history could be
1.Alcohol https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/411145
2.smoking https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6541867/
b) Please describe the ECG changes and correlate them with the patient\"s current diagnosis.
The ecg suggests: 1st ecg-irregularly irregular rythmn,normal axis, Intermittent broad qrs complexes ? ventricular escape rythmn,?idioventricular rythmn Remaining ecg-poor r wave progression with regular rythmn
c) Share an RCT that provides evidence for the efficacy of primary PTCA in acute myocardial infarction over medical management. Describe the efficacy in a PICO format. https://pubmed.ncbi.nlm.nih.gov/14522473/#:~:text=In%20the%20medical%20group%2C%2035.4,anginal%20symptoms%20and%20exercise%20times