75 YRS OLD MALE PATIENT WITH UNCONTROLLED DIABETES MELLITUS TYPE 2
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case i have seen:
A 75 year old male patient came to regular checkup in opd in view of high sugars
Patient is a known case of diabetes mellitus type II since 15 years and on medication Tab gilclazide 40 mg od
Patient had no complaints of polyuria ,nocturia,weight loss
Has normal appetite
Patient had no history of fever,cold,cough
Patient is a known case of hypertension since 10 years on medication Tab. Amolong 5 mg po od
Patient came with complaints of loosening of upper front teeth since 1 month diagnosed as Dentinal Hypersensitivity and Gingival hypertrophy ,relieved on medication
Patient had history of cva in 2018
complaint of left upper and lower limb weakness with deviation of mouth to right improved in 3 months
MRI Brain showed Acute Infarct in Lentiform Nucleus, body of caudate on right side
No complaints of nausea and vomiting
No complaints of chest pain ,palpitations,syncopal attack
No complaints of Sob,orthopnea,pnd
History of smoking since 50 years (20 beedis per day)
Alcoholic since 50 years,regular toddy drinker 90ml/day
Abstinence since 9 months
Personal history:
Appetite: normal
Bowels: regular
Bladder- normal micturition
Family history:
No history of HTN,DM,CVA CAD, asthma, in the family
General examination: patient is conscious, coherent, cooperative
Pallor is seen.
No icterus, cyanosis, clubbing,lymphadenopathy, edema
Vitals:
Temperature: 98.9F
Pulse: 80bpm
Respiratory rate:22 cpm
Bp: 130/90 mm hg
Spo2: 98% at RA
GRBS: 342 mg%
Systemic examination:
Cvs: S1 S2 heard no additional sounds or murmurs
Rs: NVBS
Abdomen: soft,non tender
Cns: higher mental functions intact
Investigations:
HBA1C:7.5%
Blood urea:64mg/dl
Serum creatinine:1.9mg/dl
Haemoglobin:10 gm/dl
Total count:10,500cells/cu.mm
Pcv-29vol%
Platelet count:2.41 lakhs/cu.mm
Normocytic Normochromic anaemia
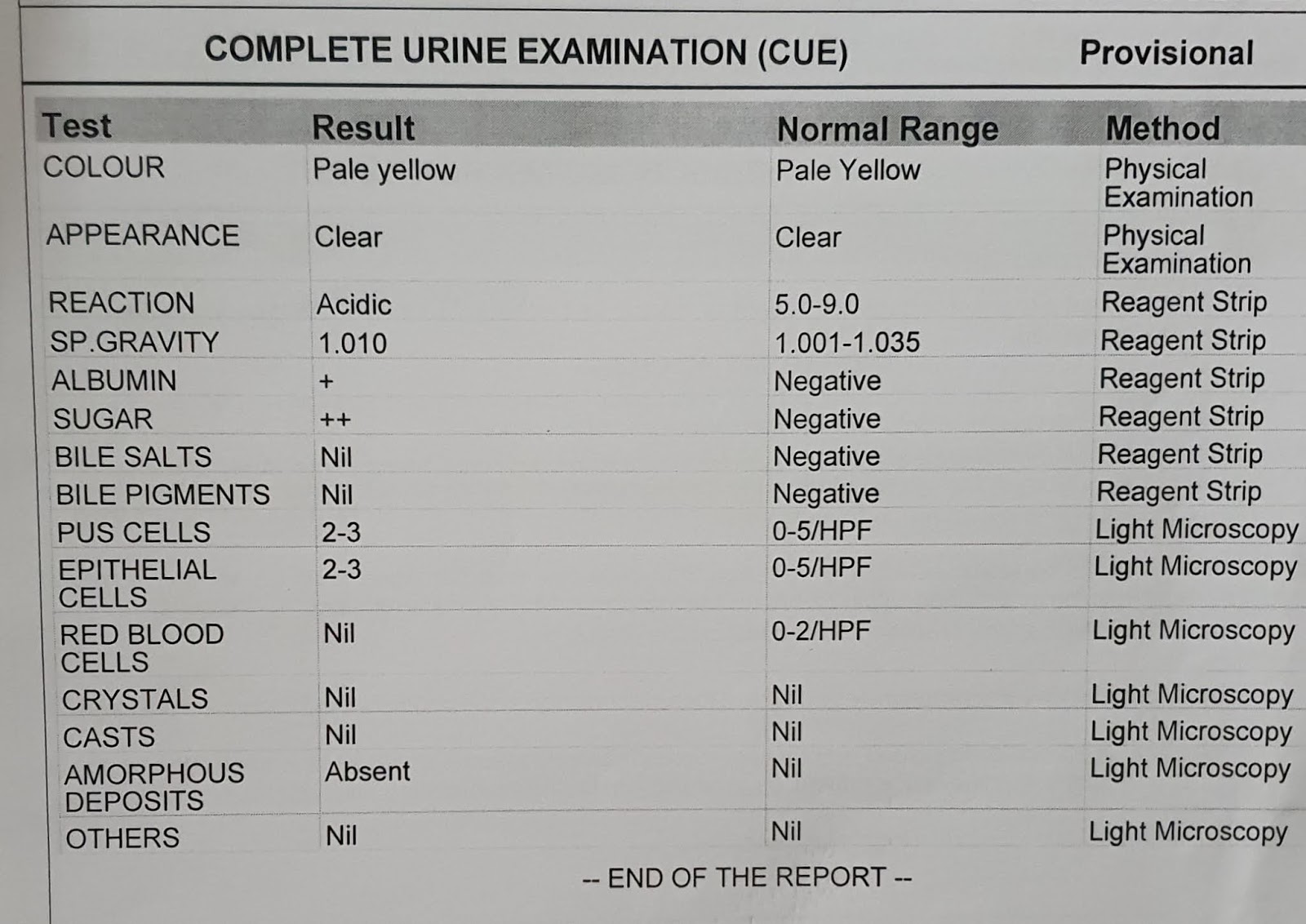
CUE:
Albumin-4+
Sugars-4+
Pus cells-3to4
Rbc-plenty
LFT:
T.Bilirubin:0.96
Direct bilirubin-0.18
AST-20
ALT-22
Alkaline phosphate-263
Total proteins-6.6
Albumin-3.7
A/G ratio-1.25
FBS-133 mg/dl
FLP:
Total cholesterol-150mg/dl
Triglycerides-313 mg/dl
HDL-51mg/dl
LDL-40 mg/dl
INVESTIGATIONS
COMPLETE URINE EXAMINATION
CHEST X RAY
TAB PAN 40 MG PO/0D @ 7 AM
TAB AMLONG 5 MG PO/OD @8AM
T. ECOSPIRIN AV 75/200MG H/S
INJ HAI S/C TID
8AM - 6U 2PM -6U 8AM -6U
INJ MIXTARD INSULIN 70/30 SC/BD
8AM -6U 2PM-× 8PM -6U
INJ CEFTRIAXONE 500 MG IV/BD
STOP ALL OHAS
TAB.MVT PO/OD
SYP. CREMAFFINE 10 ML H/S
STRICT DIABETIC DIET
BP, PR ,RR SPO2 MONITORING 6 TH HRLY
GRBS MONITORING 6 TH HRLY
8 AM - 2PM -8PM -2AM
I /O CHARTING.




 ECG
ECG